Abstract
Introduction
Philadelphia-negative MPNs are most prevalent in the older population (median age at the diagnosis above 60 years) and are rarely diagnosed in pediatrics. It is estimated that the overall incidence of MPNs in pediatric patients is around 0.82 per 100,000 patients yearly, and MPNs are approximately 100 times more common in adults than children.
Methods: We performed a systematic review following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. English literature (PubMed, SCOPUS, and Google Scholar) was searched for studies, reviews, case series, and case reports of patients with Philadelphia negative MPNs (including essential thrombocythemia, polycythemia vera, primary myelofibrosis) in the pediatric age group (< 18 years). Only studies that fulfilled WHO-2008 or 2016 criteria for MPN were included.
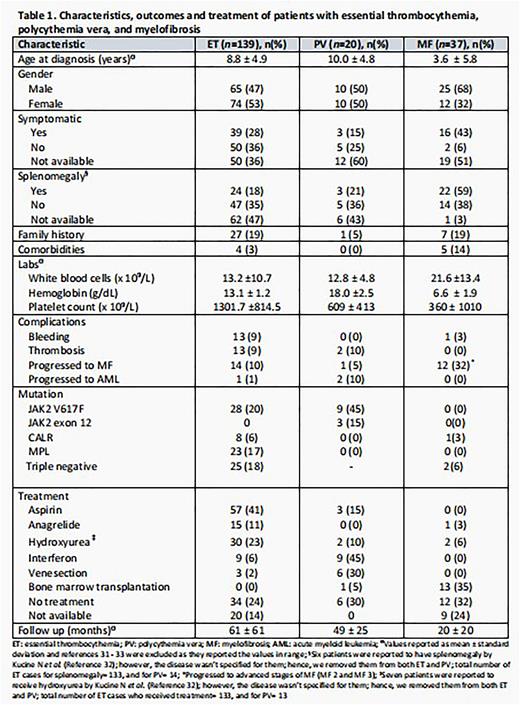
Results: We reviewed 33 articles of available published literature from 2008 to 2022 and collected data on a total of 196 patients in the pediatric population. Among the cohort of patients, 139 had essential thrombocythemia (ET), 20 had polycythemia vera (PV), and 37 had myelofibrosis (MF). Patients' clinical and biological characteristics are addressed in Table 1. The median age at the time of diagnosis for each disease varied, with 8.8 years for ET, 10 years for PV, and 3.6 years for MF. There was a variety in the blood counts at the time of diagnosis between all three diseases (Table 1).
Discussion: Based on our review, the presence of splenomegaly pediatrics with PV was not mentioned in most cases, yet around a third of the reported data have splenomegaly, matching the percentage found in adults. On the other hand, hemorrhage was not observed in pediatrics with PV, thrombosis complicated in 2 (10%) cases, and leukemic transformation was documented in 2 (10%) cases. The number of PV cases in this review is small, with only 20 reported cases, so it is challenging to get conclusions, yet the presentation and complications between adults and pediatrics are comparable, apart from a possibly higher chance for AML transformation in the pediatric population. In adults with PV, around 98% of the patients were positive for either JAK2V617F in 95% or other JAK2 mutations in 3%. While in this pediatrics review, JAK2V617F mutation was found in only 45% of the cases and JAK2 exon 12 mutation in 15%.
36% of the ET cases were asymptomatic at presentation, a number lower than that observed in adults (45%). However, thrombosis is less common in pediatrics than in adults (9% versus 21%), and bleeding as a complication from ET in pediatrics was equal to adults (9%). JAK2V617F was the most common mutation (20% of the ET patients).
Based on our review, MF cases in pediatrics are more common than PV cases in comparison with adults, in which MF is the least common. Data for pediatric patients with PMF is scarce; based on this sample of 37 patients, the percentage of symptomatic patients is higher than adults, but unlike adults, most pediatrics are presented with symptoms of cytopenia rather than constitutional symptoms, same for palpable splenomegaly where it was more reported compared to adults. The pediatric population with PMF has an entirely different mutation profile, with none of the patients in our data having JAK2V617F or MPL mutations. Interestingly in our collected data, none of the patients with PMF developed thrombosis or leukemic transformation, compared with 7% of adult patients who have documented leukemic transformation.
Conclusion: Given the rarity of MPNs in pediatrics and different characteristics compared with adults, international collaborative efforts to study MPNs in this age group are needed to understand these disorders better.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal